Monday, October 31, 2011
Most addicting substances
According to the panel of health experts consulted by Health magazine, here is their list:
1. Nicotine
2. Ice, Glass (Methamphetamine, smoked)
3. Crack
4. Crystal Meth (Methamphetamine, injected)
5. Valium (Diazepam)
6. Quaalude (Methaqualone)
7. Seconal (Secrobarbital)
8. Alcohol
9. Heroin
10. Crank (Amphetamine oral)
11. Cocaine
12. Caffeine
13. PCP
14. Marijuana
15. Ecstasy
16. Psilocybine Mushrooms
17. LSD
18. Mescaline
Pannus
A Panniculus is a medical term describing a dense layer of fatty tissue growth, consisting of subcutaneous fat in the lower abdominal area.[1] It can be a result of obesity and can be mistaken for a tumor or hernia. Abdominal panniculus can be removed during abdominal panniculectomy, a type of abdominoplasty. A panniculus can also be the result of loose tissues after pregnancy or massive weight loss.[2]
[edit] Grading of abdominal panniculiGrade 1
Panniculus barely covers the hairline and mons pubis but not the genitalia.
Grade 2
Extends to cover the genitalia.
Grade 3
Extends to cover the upper thigh
Grade 4
Extends to cover the mid thigh.
Grade 5
Extends to cover the knees or beyond.
Wednesday, September 28, 2011
Tips from a friend in clinical rotations
Wednesday, July 27, 2011
some lists today
1. Chloremphenicol
2. Vinblastine
3. AZT
4. Benzene
Viral causes:
1. Parvovirus B19
2. Hep C
3. Hep E
7 Drugs that can cause Neutropenia and cause agranulocytosis*
1. Carbamazapine*
2. Colchicine
3. Clozapine*
4. Propylthiouracil
5. Methimazole
6. Dapsone
7. Ticlopidine*
The Herpes viruses
HHV1 oral
HHV2 genital
HHV3 varicella
HHV4 EBV
HHV5 CMV
HHV6 Roseola
HHV7 Pityriasis
HHV8 Kaposi
Saturday, May 28, 2011
Rinne and Weber tests
In a normal ear, air conduction (AC) is better than bone conduction (BC)
AC > BC, and this is called a positive Rinne.
In conductive hearing loss, bone conduction is better than air
BC > AC, a negative Rinne.
WEBER'S TEST: In the Weber test a tuning fork (either 256 or 512 Hz) is struck and the stem of the fork is placed on the top of the patient's skull - equal distance from the patient's ears, in the middle of the forehead - equal distance from the patient's ears or above the upper lip over the teeth. The patient is asked to report in which ear the sound is heard louder.
Weber without lateralization & Rinne both ears AC>BC = Normal hearing.
HOW TO USE THE TESTS:
Weber Lateralizes Left & Rinne both ears AC > BC = senorinerual loss Right ear
Weber Lateralizes Right & Rinne both ears AC > BC = sensorineural loss Left ear
Rinne Left BC>AC & Weber's lateralized to the left = conductive loss on the left
Rinne Right BC>AC & Weber's lateralized to the right = conductive loss on the right
Wednesday, March 23, 2011
tips for clinicals
buya self-learning EKG text book
the name of the game is to impress people in clinicals
Kochar's clinical medicine for students, it is the first step of reading for ur pt
ACP medicine volume 1 david c dale daniel d federman 3rd edition
read abt ur pt everyday
write it down in the little book and later look it up in the big book
read for understandning not for fact memorization
this is also how you will learn to do life long learning
how to get an inside track
use ur electives
choose a reasonable site
work very hard do way more than what is expected
goal: to get your attending to write a glowing assesment/recommendation
name recognition bwyour attaending and the program director is the key
avoid multiple attempts to pass usmle1
dont use illict drugs ever or stop
be very careful w alcohol a dwi can ruin your career
get along in ur clerkships be a team player you cant cover urpatient 24/7
if you have a disordered personality, hide it or switch professions now
show up, be ontime, be prepared
stop using digital social media
evenbe careful what u write in email
dont like to pts , to attending, or to collegeuas
dont write orders or write anything in the chart that you dont understand, dont be a scribe
Tuesday, March 22, 2011
IL-2, IL-3, IL-4
IL-3: Secreted by activated T cells. Supports the growth and differentiation of bone marrow stem cells. Has fucntion similar to GM-CSF. Stimulates bone marrow.
IL-4: Secreted by Th2 cells. Promotes growth of B cells. Enhances class switching to IgE and IgG. Induces generic T-helper cell to become Th2 cell. IL-4 stimulates IgE and IgG production.
Corpus Callosum
Test your corpus callosum
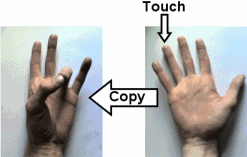 I’ve just discovered a wonderfully simple finger touch procedure that can test the function of your corpus callosum, a key brain structure that connects the two cortical hemispheres.
I’ve just discovered a wonderfully simple finger touch procedure that can test the function of your corpus callosum, a key brain structure that connects the two cortical hemispheres.
It is called the ‘cross lateralization of fingertips test’ and was used in a 1991 study by Kazuo Satomi and colleagues.
It relies on the fact that different hemispheres are responsible for the movements and sensations from each hand.
In other words, each hand is connected to a different side of the brain, and, to allow you to co-ordinate both hands, the brain passes information between the two sides by using the corpus callosum.
The corpus callosum is the largest structure in the brain and works like a huge bundle of white matter ‘cables’, connecting different areas.
If this structure gets damaged, a patient might have trouble with coordinating their hands, preventing them from matching sensations on one hand with movement on the other, because the information doesn’t get to where it’s needed.
The test works like this: you need to ask someone to close their eyes and put their hands face up.
You then touch one of their fingertips with a pencil, and with the opposite hand the participant needs to touch the corresponding finger with thumb of the same hand.
For example, if you touched their right ring finger, they would need to touch their left ring finger with their left thumb, as shown in the diagram above.
You need to do this on both hands, with them always touching the corresponding finger on the opposite hand.
It’s important that the person keeps their eyes closed, because as soon as they look, they get information from the eyes, which goes to both hemispheres.
Patients who have damage to the corpus callosum (either because of acquired damage or because it just hasn’t developed) usually can’t do this test, because of the disruption in communication between the two hemispheres of the brain.
Of course, just to be sure its not a problem with movement or sensation in one hand only, the patient is also asked to do another quick test where they’re asked touch the exact finger you just touched.
For this part, the sensation and movement happen in the same hand, so information doesn’t need to cross the corpus callosum.
The test was shown to me by Dr Emma Barkus, who researches what neurological tests can tell us about psychosis and unusual experiences.
One Comment
The test you describe for the corpus callosum has been around since the 1970′s. It is called Tactile Localization. I have used it for 35 years as you describe it except that I make the student hold the hand behind him that I will touch so I can be sure he hasn’t seen it. I have never had it fail to pick out dyslexia. The beauty of it is that it doesn’t cost a thing and can be done by anybody. A person with poor reading, a good IQ and a few mistakes on TL is a guarantee of dyslexia.
And it is free! Dorothy van den Honert
Hyporeflexia
Gastroenteritis
Gastroenteritis (also known as gastric flu, stomach flu, stomach virus, although unrelated to influenza) is inflammation of the gastrointestinal tract, involving both the stomach and the small intestine and resulting in acute diarrhea and vomiting. It can be transferred by contact with contaminated food and water. The inflammation is caused most often[citation needed] by an infection from certain viruses or less often[citation needed] by bacteria, their toxins (e.g. SEB), parasites, or an adverse reaction to something in the diet or medication. Current death rates have come down significantly to approximately 1.5 million deaths annually in the year 2000, largely due to the global introduction of oral rehydration therapy[1] and is a leading cause of death among infants and children under 5.[2]
At least 50% of cases of gastroenteritis due to foodborne illness are caused by norovirus.[3] Another 20% of cases, and the majority of severe cases in children, are due to rotavirus. Other significant viral agents include adenovirus[4] and astrovirus.
Different species of bacteria can cause gastroenteritis, including Salmonella, Shigella, Staphylococcus, Campylobacter jejuni, Clostridium, Escherichia coli, Yersinia, Vibrio cholerae, and others. Some sources of the infection are improperly prepared food, reheated meat dishes, seafood, dairy, and bakery products. Each organism causes slightly different symptoms but all result in diarrhea. Colitis, inflammation of the large intestine, may also be present.
Risk factors include consumption of improperly prepared foods or contaminated water and travel or residence in areas of poor sanitation. It is also common for river swimmers to become infected during times of rain as a result of contaminated runoff water.[5]
Contents[hide] |
[edit] Classification
Infectious gastroenteritis is caused by a wide variety of bacteria and viruses. It is important to consider infectious gastroenteritis as a diagnosis per exclusionem. A few loose stools and vomiting may be the result of systemic infection such as pneumonia, septicemia, urinary tract infection and even meningitis. Surgical conditions such as appendicitis, intussusception and, rarely, even Hirschsprung's disease may mislead the clinician. Endocrine disorders (e.g. thyrotoxicosis and Addison's disease) are disorders that can cause diarrhea. Also, pancreatic insufficiency, short bowel syndrome, Whipple's disease, coeliac disease, and laxative abuse should be excluded as possibilities.[6]
[edit] Bacterial gastroenteritis
For a list of bacteria causing gastroenteritis, see above. Pseudomembranous colitis is an important cause of diarrhea in patients often recently treated with antibiotics. Traveler's diarrhea is usually a type of bacterial gastroenteritis.
If gastroenteritis in a child is severe enough to require admission to a hospital, then it is important to distinguish between bacterial and viral infections. Bacteria, Shigella and Campylobacter, for example, and parasites like Giardia can be treated with antibiotics.
[edit] Viral gastroenteritis
Viruses causing gastroenteritis include rotavirus, norovirus, adenovirus and astrovirus. Viruses do not respond to antibiotics and infected children usually make a full recovery after a few days.[7] Children admitted to hospital with gastroenteritis routinely are tested for rotavirus A to gather surveillance data relevant to the epidemiological effects of rotavirus vaccination programs.[8][9] These children are routinely tested also for norovirus, which is extraordinarily infectious and requires special isolation procedures to avoid transmission to other patients. Other methods, electron microscopy and polyacrylamide gel electrophoresis, are used in research laboratories.[10][11]
[edit] Symptoms and signs
Gastroenteritis often involves stomach pain or spasms, diarrhea and/or vomiting, with noninflammatory infection of the upper small bowel, or inflammatory infections of the colon.[12][6][13][14]
The condition is usually of acute onset, normally lasting 1–6 days, and is self-limiting.
- Nausea and vomiting
- Diarrhea
- Loss of appetite
- Fever
- Headaches
- Abnormal flatulence
- Abdominal pain
- Abdominal cramps
- Bloody stools (dysentery - suggesting infection by amoeba, Campylobacter, Salmonella, Shigella or some pathogenic strains of Escherichia coli[4])
- Fainting and Weakness
- Heartburn
The main contributing factors include poor feeding in infants. Diarrhea is common, and may be followed by vomiting. Viral diarrhea usually causes frequent watery stools, whereas blood stained diarrhea may be indicative of bacterial colitis. In some cases, even when the stomach is empty, bile can be vomited up.
A child with gastroenteritis may be lethargic, suffer lack of sleep, run a low fever, have signs of dehydration (which include dry mucous membranes), tachycardia, reduced skin turgor, skin color discoloration, sunken fontanelles, sunken eyeballs, darkened eye circles, glassy eyes, poor perfusion and ultimately shock.
[edit] Diagnosis
Gastroenteritis is diagnosed based on symptoms, a complete medical history and a physical examination. An accurate medical history may provide valuable information on the existence or inexistence of similar symptoms in other members of the patient's family or friends. The duration, frequency, and description of the patient's bowel movements and if they experience vomiting are also relevant and these question are usually asked by a physician during the examination. [15]
No specific diagnostic tests are required in most patients with simple gastroenteritis. If symptoms including fever, bloody stool and diarrhea persist for two weeks or more, examination of stool for Clostridium difficile may be advisable along with cultures for bacteria including Salmonella, Shigella, Campylobacter and enterotoxic Escherichia coli. Microscopy for parasites, ova and cysts may also be helpful.[citation needed]
A complete medical history may be helpful in diagnosing gastroenteritis. A complete and accurate medical history of the patient includes information on travel history, exposure to poisons or other irritants, diet change, food preparation habits or storage and medications. Patients who travel may be exposed to E. Coli infections or parasite infections contacted from beverages or food. Swimming in contaminated water or drinking from suspicious fresh water such as mountain streams or wells may indicate infection from Giardia - an organism found in water that causes diarrhea.
Food poisoning must be considered in cases when the patient was exposed to undercooked or improperly stored food. Depending on the type of bacteria that is causing the condition, the reactions appear in 2 to 72 hours. Detecting the specific infectious agent is required in order to establish a proper diagnosis and an effective treatment plan.
The doctor may want to find whether the patient has been using broad-spectrum or multiple antibiotics in their recent past. If so, they could be the cause of an irritation of the gastrointestinal tract.
During the physical examination, the doctor will look for other possible causes of the infection. Conditions such as appendicitis, gallbladder disease, pancreatitis or diverticulitis may cause similar symptoms but a physical examination will reveal a specific tenderness in the abdomen which is not present in gastroenteritis.
Diagnosing gastroenteritis is mainly an exclusion procedure. Therefore in rare cases when the symptoms are not enough to diagnose gastroenteritis, several tests may be performed in order to rule out other gastrointestinal disorders. These include rectal examinations, complete blood count, electrolytes and kidney function tests. However, when the symptoms are conclusive, no tests apart from the stool tests are required to correctly diagnose gastroenteritis especially if the patient has traveled to at-risk areas.
[edit] Prevention
Since 2000, the implementation of a rotavirus vaccine has decreased the number of cases of diarrhea due to rotavirus in the United States.[16]
Gastroenteritis may be prevented through immunization. [17] The U.S. Food and Drug Administration approved in 2006 a rotavirus vaccine called Rotateq that may be given to infants aged 6 to 32 weeks to prevent getting infected with viral gastroenteritis. [18] The vaccines may however have side effects that are similar to the mild flu symptoms.
Different types of vaccinations are available for Salmonella typhi and Vibrio cholera and which may be administered to people who intend traveling in at-risk areas. However, the vaccines that are currently available are effective only on rotavirual gastroenteritis.
Doctors recommend that food be properly cooked and stored to prevent gastroenteritis. Avoid suspect food or drink. Thoroughly wash both hands before eating and after using the bathroom or changing diapers. Viral gastroenteritis is a highly contagious disease and thus avoiding crowded spaces such as markets, theaters or shopping centers may also help in preventing infection for those who have weak resistance. Bleaching soiled laundry and household surfaces may help prevent spreading bacteria. [19]
[edit] Management
Gastroenteritis is usually an acute and self-limited disease that does not require pharmacological therapy.[20] The objective of treatment is to replace lost fluids and electrolytes. Oral rehydration is the preferred method of replacing these losses in children with mild to moderate dehydration.[21] Metoclopramide and ondansetron however may be helpful in children.[22]
[edit] Rehydration
The primary treatment of gastroenteritis in both children and adults is rehydration, i.e., replenishment of water and electrolytes lost in the stools. This is preferably achieved by giving the person oral rehydration therapy (ORT) although intravenous delivery may be required if a decreased level of consciousness or an ileus is present.[23][24] Complex-carbohydrate-based oral rehydration therapy such as those made from wheat or rice may be superior to simple sugar-based ORS.[25]
Sugary drinks such as soft drinks and fruit juice are not recommended for gastroenteritis in children under 5 years of age as they may make the diarrhea worse.[20] Plain water may be used if specific ORS are unavailable or not palatable.[20]
[edit] Diet
It is recommended that breastfed infants continue to be nursed on demand and that formula-fed infants should continue their usual formula immediately after rehydration with oral rehydration solutions. Lactose-free or lactose-reduced formulas usually are not necessary.[26] Children receiving semisolid or solid foods should continue to receive their usual diet during episodes of diarrhea. Foods high in simple sugars should be avoided because the osmotic load might worsen diarrhea; therefore substantial amounts of soft drinks, juice, and other high simple sugar foods should be avoided.[26] The practice of withholding food is not recommended and immediate normal feeding is encouraged.[27] The BRAT diet (bananas, rice, applesauce, toast and tea) is no longer recommended, as it contains insufficient nutrients and has no benefit over normal feeding.[28]
[edit] Medications
- Antiemetics
Antiemetic drugs may be helpful for vomiting in children. Ondansetron has some utility with a single dose associated with less need for intravenous fluids, fewer hospitalizations, and decreased vomiting.[29][30][31] Metoclopramide also might be helpful.[32] However there was an increased number of children who returned and were subsequently admitted in those treated with ondansetron.[33] The intravenous preparation of ondansetron may be given orally.[34]
- Antibiotics
Antibiotics are not usually used for gastroenteritis, although they are sometimes used if symptoms are severe (such as dysentery)[35] or a susceptible bacterial cause is isolated or suspected.[36] If antibiotics are decided on, a fluoroquinolone or macrolide is often used.[13] Pseudomembranous colitis, usually caused by antibiotics use, is managed by discontinuing the causative agent and treating with either metronidazole or vancomycin.[13][14]
- Antimotility agents
Antimotility drugs have a theoretical risk of causing complications; clinical experience, however, has shown this to be unlikely.[6][13] They are thus discouraged in people with bloody diarrhea or diarrhea complicated by a fever.[12] Loperamide, an opioid analogue, is commonly used for the symptomatic treatment of diarrhea.[13] Loperamide is not recommended in children as it may cross the immature blood brain barrier and cause toxicity. Bismuth subsalicylate (BSS), an insoluble complex of trivalent bismuth and salicylate, can be used in mild-moderate cases.[6][13]
- Antispasmotics
Butylscopolamine (Buscopan) is useful in treating crampy abdominal pain.[37]
[edit] Alternative medicine
- Probiotics
Some probiotics have been shown to be beneficial in preventing and treating various forms of gastroenteritis.[28] They reduce both the duration of illness and the frequency of stools.[38] Fermented milk products (such as yogurt) also reduce the duration of symptoms.[39]
- Zinc
The World Health Organization recommends that infants and children receive a dietary supplement of zinc for up to two weeks after onset of gastroenteritis.[40] A 2009 trial however did not find any benefit from supplementation.[41]
[edit] Complications
Dehydration is a common complication of diarrhea. It can be made worse with the withholding fluids or the administration of juice / soft drinks.[42] Malabsorption of lactose, the principal sugar in milk, may occur. Though it may increase the diarrhea,[43] however, mothers should continue breastfeeding.
[edit] Epidemiology

Every year worldwide rotavirus in children under 5, causes 111 million cases of gastroenteritis and nearly half a million deaths. 82% of these deaths occur in the world's poorest nations.[44]
In 1980 gastroenteritis from all causes caused 4.6 million deaths in children with most of these occurring in the third world.[14] Lack of adequate safe water and sewage treatment has contributed to the spread of infectious gastroenteritis. Current death rates have come down significantly to approximately 1.5 million deaths annually in the year 2000, largely due to the global introduction of oral rehydration therapy.[45]
The incidence in the developed world is as high as 1-2.5 cases per child per year[citation needed] and is a major cause of hospitalization in this age group.
Age, living conditions, hygiene and cultural habits are important factors. Aetiological agents vary depending on the climate. Furthermore, most cases of gastroenteritis are seen during the winter in temperate climates and during summer in the tropics.[14]
[edit] History
Before the 20th century, the term "gastroenteritis" was not commonly used. What would now be diagnosed as gastroenteritis may have instead been diagnosed more specifically as typhoid fever or "cholera morbus", among others, or less specifically as "griping of the guts", "surfeit", "flux", "colic", "bowel complaint", or any one of a number of other archaic names for acute diarrhea.[46] Historians, genealogists, and other researchers should keep in mind that gastroenteritis was not considered a discrete diagnosis until fairly recently.
U.S. President Zachary Taylor died of gastroenteritis on July 9, 1850.[47]
Danazol
Danazol is a derivative of the synthetic steroid ethisterone, a modified testosterone. Also known as 17alpha-ethinyl testosterone. Before becoming available as a generic drug, Danazol was marketed as Danocrine in the United States. It was approved by the U.S. Food and Drug Administration (FDA) as the first drug to specifically treat endometriosis in the early 1970s.[1] Although effective for endometriosis, its use is limited by its masculinizing side-effects.[2] Its role as a treatment for endometriosis has been largely replaced by the GnRH agonists.
Contents[hide] |
[edit] Chemistry
The agent is fat-soluble. It is an isoxazole of testosterone with isolated weak androgenic activity and no estrogenic or progestagenic effects.[1]
[edit] Method of action
Danazol inhibits ovarian steroidogenesis resulting in decreased secretion of estradiol and may increase androgens. Pituitary hormones are largely unaffected although luteinizing hormone (LH) may be slightly elevated.[3]
[edit] Indications
Danazol has been used - mostly off-label - for other indications, namely in the management of menorrhagia, fibrocystic breast disease, immune thrombocytopenic purpura, breast pain (mastodynia) and hereditary angioedema.[4] Though danazol prevents pregnancy, it is not licenced for use as a contraceptive agent.
Although not currently a standard treatment for menorrhagia, danazol has resulted in significant relief in young women with menorrhagia in a study, and, because of a lack of significant adverse effects, it was proposed as an alternative treatment.[5]
[edit] Side-effects
Androgenic side effects are of concern, because in sensitive female patients, danazol can enhance unwanted hair growth, leading to hirsutism. On rare occasion, it can deepen the voice. Other possible side effects include acne and oily skin. Because danazol is metabolized by the liver, it cannot be used by patients with liver disease, and in patients receiving long-term therapy, liver function must be monitored on a periodic basis. Some patients who use danazol experience weight gain and fluid retention. Due to these limitations, danazol is seldom prescribed continuously beyond six months.
The use of danazol for endometriosis has been linked to an increased risk of ovarian cancer.[6] Patients with endometriosis have specific risk factors for ovarian cancer so this may not apply for other uses.
Danazol has, like most other androgenic agents, been linked with an increased risk of liver tumors. These are generally benign.[7]
Unlike GnRH agonists, danazol does not induce osteoporosis. Also, symptoms of hot flushes tend to be less common or severe.
[edit] Contraindications
Danazol is contraindicated in pregnancy because it could masculinize a female fetus.
Objective of MeDerp
- Post educational objectives from incorrect questions
- Post diagrams, charts, and helpful learning tools for information
- Post mnemonics that help for memorization
Ok, let's do this!
